Obesity: Metabolic Dysfunction and Diet
By: Eric Lieberman MD, Jonathan Kahan MD
What you need to know:
We can estimate metabolic dysfunction in multiple ways. Metabolic dysfunction leads to most cardiovascular diseases.
The combination of eating processed foods and lack of exercise is the root cause of metabolic dysfunction
A processed food is wrapped in plastic, has a nutrition label, makes a health claim, lasts a long time and has ingredients not found in a standard kitchen. There are relative grades of processing. The less processed the food the better. The dose makes the poison.
There are classes of medications that can aid in weight loss which may be an option for you.
The progression goes from overweight →
obese →
metabolic dysfunction →
insulin resistance →
prediabetes →
5. diabetes. Patients can move up or down this scale. You can be normal weight and have metabolic dysfunction or obese and have a normal metabolism. Metabolism changes very little as we age.
Why care about obesity?
Obesity affects more than 40% of Americans today and is a key driver of several disease processes that impact cardiovascular (CVD) risk1. This number is rising yearly.
Obesity means I have metabolic issues, right? It's like having diabetes, right?
Metabolic abnormalities have a variety of manifestations. They occur on a spectrum from obesity, metabolic syndrome, insulin resistance, prediabetes and diabetes. There are different definitions for each of these.
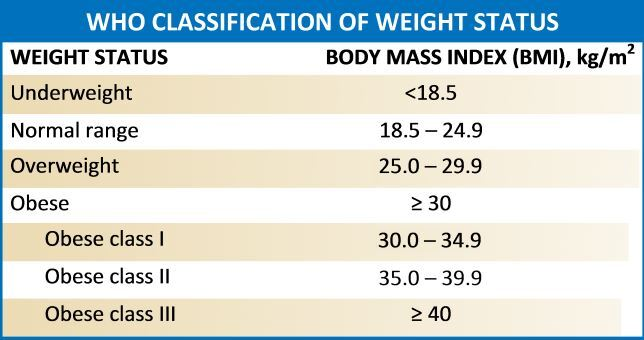
Obesity = Elevated body mass index (BMI) which is a ratio of your weight over your height squared (kg/m2):
Stahl, Jonathan M., and Sandeep Malhotra. “[Figure, BMI Chart with Obesity Classifications...].” Www.ncbi.nlm.nih.gov, July 2022
Note: This does not distinguish between muscle, fat, bone or body composition in any way2
2. Insulin Resistance is a precursor to prediabetes and diabetes. To test accurately would require a glucose clamp, however, we can estimate using the below calculation (Homeostatic Model of Insulin Resistance aka HOMA IR):
HOMA IR = fasting glucose (mg/dL) X fasting insulin (mU/L) / 405
A value >2 = Insulin Resistance3
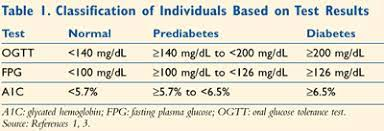
3. Pre Diabetes (preDM) / Diabetes (DM) = A further continuum of metabolic dysfunction, diabetes is divided into type 1 (where antibodies attack the pancreas and a patient will require insulin) and type 2 diabetes where a patient’s lifestyle leads to the disease. Type 1 is outside the scope of this book whereas type 2 is exactly what this book is about (and much more common). There are 3 ways to test to see if a patient has preDM or DM. This is done either with performing an oral glucose tolerance test (OGTT), testing fasting blood glucose, or measuring hemoglobin A1c. OGTT is performed by first testing your blood sugar (aka glucose) level prior to drinking 75 grams of glucose, then testing it one hour and then two hours after. Hemoglobin A1c measures your 3-month average blood glucose.
Note: HbA1c measures sugar molecules attached to red blood cells. Sugar is sticky, and this is partly how blockages occur in the smallest arteries (ie. microvascular) of the body.
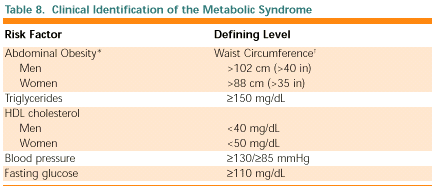
4. Metabolic Syndrome (X) = a cluster of three out of five (3/5) of the following conditions(5):
Note: metabolic syndrome are signs that a patient has impaired metabolism that can lead to diseases of the arteries
What is food?
Food Definition6: material containing or consisting of carbohydrates, fats, and proteins used in the body of an animal to sustain growth, repair, and to furnish energy and other vital processes (Webster’s dictionary).
****Most “food” in the standard American diet (SAD) aka the Western diet does not meet this definition as they do not perform the latter processes****
What is metabolism?
Metabolism7: the process of ingesting food, which is made up of protein, fat, carbohydrates, vitamins/minerals and water and breaking them down into amino acids (protein), free fatty acids (fat), glucose (carbohydrates). This is the catabolism part of metabolism. The next process is anabolism, which is using the basic building blocks of amino acids etc to make up components of the cell eg. enzymes (proteins), membranes (fats) and ATP (glucose/fats). [this is a simplified definition]. Note metabolism does not change from the age 20-60, then decreases in efficacy by approximately 0.7% per year after the age of 60 (mainly through loss of muscle mass). The way we calculate our metabolism technically is through the Total Daily Energy Expenditure (TDEE). The components of this are our Basal Metabolic Rate (BMR, our true baseline metabolic rate to stay alive), our Exercise and Non-Exercise Activity Thermogenesis (EAT and NEAT), and the Thermic Effect of Food (TEF). We cover each component in this section.
Can I be obese but metabolically healthy?
Yes! About 30% of obese patients (as defined by BMI, see above) are considered metabolically healthy8. While definitions vary, generally these are patients with normal HOMA-IR (<2, see above) and do not meet Metabolic Syndrome X criteria. HOWEVER, obesity is the root cause of a multitude of other diseases including obstructive sleep apnea (which causes hypertension and fatigue secondary to a buildup of carbon dioxide which is a poison), hypertension, joint and back pain, elevated cholesterol, and coronary artery disease and strokes (this is not an exhaustive list of issues). The higher the weight, the higher the chance of becoming metabolically unhealthy. This is related to the 5 different types of fat and the consequences of fat distribution (see below): Of note, you can also be normal weight but have high levels of fat around the organs and body, leading to metabolic dysfunction as well.
What does insulin do in the body? Why is insulin resistance bad?
In response to ingesting (mainly) carbohydrates, insulin is secreted from the pancreas. This causes glucose (sugar) to be taken up in the muscles (via GLUT4 transporter) and liver (to store sugar and stop making new glucose). It also enhances amino acid (protein) uptake into tissues, and causes the fat cells (remember 5 types) to start to take up free fatty acids.
When there is an excess of insulin stimulation (such as excess calories, processed foods, carbs etc, or lack of muscle or liver damage) the peripheral tissues stop responding to the chronically elevated insulin levels. In the fat cells this manifests as free fatty acid spillover, while in the liver this leads to continued glucose production (which damages blood vessels) and lipid production (leading to fatty liver). In the muscles there is a reduction in the GLUT4 transporter while in the kidneys it leads to sodium retention (leading to high blood pressure) and increased internal pressure eventually creating renal damage. In the brain it leads to neurodegenerative changes (leading to Alzheimer’s dementia) and dysregulation of the appetite signals in the brain via leptin.
Of note, ingesting fat does not lead to an increase in insulin. Ingesting protein does lead to an increase in insulin, but also increases glucagon which mitigates the effects of insulin (by allowing fat cells to use/store more fatty acids and by letting the liver return to normal sugar/lipid production). Carbohydrates lead to a pure increase in insulin without glucagon effect. We will next go over the different types of fat cells and then finalize the whole picture by going through what those free fatty acids do in the body once in the blood stream. See the next two paragraphs:
Are there different types of body fat?
Yes! There are 5 main types of fat on a person's body (this is a simplification)9:
Subcutaneous fat (white fat)10, fat that is present around the hips, butt and thighs. Humans can store about ~20 lbs of fat in these areas. These fat cells accept free fatty acids (FFA) and store them within cells in vacuoles (think giant bubbles). When these bubbles burst, they spill FFA into the bloodstream and surrounding tissues which can lead to metabolic syndrome. The way this happens is by FFA entering muscle cells causing sugar regulation dysfunction (muscle is the main regulator of sugar in the body!).
Visceral (VAT) fat11: This is fat that surrounds organs or has direct access to organs. The most concerning examples of this are abdominal fat and epicardial (beside the heart) fat. Whether the body makes visceral vs. subcutaneous fat appears to be poorly understood, and is a combination of age, genetics, hormonal (estrogen, and testosterone) and the lifestyle factors (cortisol) listed in this book. Alcohol may have a predilection for the development of visceral fat.
Visceral fat is hormonally active and is a major driver of inflammation. The mechanism where visceral fat leads to metabolic syndrome is via cytokines (signaling chemicals) that increase inflammation in the body, vessels walls and organs, leading to metabolic dysfunction and atherosclerosis (plaque in the arteries of the heart).
Free fatty acids (FFA)/cytokines from visceral fat in the abdomen goes straight to the liver via the portal vein (think super highway), causing nonalcoholic fatty liver disease (NAFLD). Epicardial fat sits directly on top of the heart12. We can see and measure epicardial fat on ultrasounds of the heart. This type of fat damages the heart in the same way abdominal fat damages the liver. There is a strong correlation between epicardial fat and heart attacks.
3. Organ fat13, i.e. fat that develops within the organs themselves. Examples of this include fat deposition within the liver. You need very little of this fat to cause serious issues. Saturated fat and excess sugar, especially fructose, gets converted in the liver to FFA and stored as triglycerides (TG), leading to the development of fatty liver disease and inflammation.
4. Intramuscular fat54. Intramuscular fat aka intramyocellular lipids (IMCL) offer an important energy source in the form of FFA during endurance activities. Regular endurance exercise improves the muscle capacity to use this energy source. Too much intramuscular fat however leads to insulin resistance, metabolic syndrome, diabetes (muscles are the main regulators of sugar) oxidative stress and muscle toxicity.
5. Brown fat55. Limited in adults, brown fat is activated during cold exposure as a way to heat the body and increase the metabolic rate. Chronic cold exposure can convert white to brown fat which can improve insulin sensitivity, help with weight management. Obesity leads to less brown fat overall.
How does obesity lead to metabolic syndrome?
When we consume excess foods that lead to metabolic derangement eg. processed foods, we accumulate excess energy in the form of free fatty acids (FFA)/sugars into the types of fat listed above14. We saw above how chronic excess insulin leads to insulin resistance in multiple organs. If the FFA is stored in subcutaneous fat, then it can spill over leading to inflammation, toxicity, mitochondrial dysfunction and insulin resistance. If the FFA are stored in visceral fat (remember a number of factors play into why excess energy goes into subcutaneous vs. visceral fat including age, genetics etc.) then it can directly damage the organs it is attached to (epicardial fat in the case of the heart, abdominal fat via the portal vein superhighway in the case of the liver).
Once these organs uptake the fat e.g. heart, muscle, liver, the FFA cause direct damage to a number of processes leading to overt disease. In the liver they can be stored as triglycerides which cause all the problems discussed above, in the muscle they impair glucose transport (our muscles are the main sinks for sugar) leading to metabolic dysfunction and some are incorporated into the lipoproteins which cause damage to the vascular walls themselves (leading to inflammation and plaque development). Excess sugars can go to the liver where they are converted to triglycerides which then follows the exact mechanisms as above, or leads to chronically elevated insulin which can lead to insulin resistance on its own.
So what causes Obesity AKA Metabolic Syndrome AKA prediabetes AKA diabetes?
Obesity etc. is a modern problem, rising to epidemic proportions in the 1970’s and spreading throughout the rest of the world. The rise of metabolic syndrome and cardiovascular disease correlates with the move to processed and ultra processed foods in combination with lack of activity15,16. This leads to most cardiovascular diseases which as previously shown is the number one cause of morbidity and mortality in the world.
What is processed food and why is it bad?
Humans have been processing food for millennia. You can change food without changing macros, but by changing characteristics you can take a food from natural to ultra processed (think apple to applesauce to fruit strip)17. Note, I have not changed the macro components at all. The protein, fat and carbohydrates are exactly the same. However, this new form of food has significant consequences. The more processing done to a food, the faster it speeds through our digestive system, which causes us to eat more. Additionally, they are more calorie dense and contain obesogens (chemicals that cause obesity). Furthermore, fiber and other nutrients have an architecture, which are destroyed in the process (more on that later)18. It is very important to understand that this is unrelated to macros. It is not about high protein, low carb, fat free, high fiber etc. it is about how close to how the food would exist in nature.
Example: In Keto 1.0 (where no keto friendly i.e. zero carb processed foods were available), people lost a lot of weight and corrected the metabolic issues plaguing them. The main problem with Keto 1.0 was that it was not sustainable in the long term. Now there is keto 2.0 which contains keto pizza, ice cream etc. and people who eat these foods have the same problems as people who eat processed foods despite eating zero carbs.
How can I tell what is processed food?
Approximately 80% of food in our grocery stores in the Western world is processed and our nutritional labels do little to tell us which foods are processed or what was done to them. In general, if it comes in a plastic wrapper or bag it is processed. If it contains ingredients not found in a typical kitchen it is ultra processed. If it makes a health claim such as “high in fiber/vitamins” there is a reasonable chance it is processed. If it has multiple ingredients it is processed. If it has ANY added sugars or sweeteners it is processed (note, there are multiple words for sugar, and on food labels they separate them out, but when added together they make up a large percentage of that food). If a food lasts for a long time (e.g. bread with expiration dates of months, cold cuts etc.) it is highly processed. This is also true if a food is ready to eat (e.g. instant noodles, hot dogs, microwaveable meals).
There is a classification system called NOVA19 which helps break food into 4 categories of processed foods, although at the time of this writing it does not contain every brand/food available. Class 1 is unprocessed/minimally processed without added salt, sugar and oil. Class 3 are foods that have salt, sugar or oil added for preservation, flavor enhancement or to prolong shelf life (eg. sodium >140 mg/serving, sugar equal to 5-10% of product weight, or oil used in preservation). Note that Nova Class 4 is ultra processed and is the category that causes the most metabolic dysfunction. See the appendix for a list of food categories to avoid. There is a free app called Yuka® which you can scan almost every product to see if it has hazardous chemicals, although at the time of this writing it does not classify foods based on NOVA or state their processing. Note the nutrition label contains very little about what was actually done to our food (and serves as a warning that the food is probably processed). A large proportion of restaurant/fast food is highly processed regardless of health claims.
Is a calorie a calorie? Are calories important in weight loss?
A calorie is the amount of heat needed to raise the temperature of 1 gram of water by 1 degree Celsius. We use calories as an estimate for how much energy is in food. Weight loss comes down to running a deficit of calories under all circumstances. The only thing that changes is the method to achieve this deficit. To put things another way, you can not lose weight/fat if you eat more calories than you use. Note also that the calories we consume do not always equal the calories absorbed. For example, if you eat 100 calories of almonds you will absorb only 70 calories, the rest goes to your gut microbiome (more on that later)21. Additionally, there is the thermal effect of food (TEF), where it takes more energy to break down a whole food than a processed food, or to heat a food up for processing, such as drinking cold water. Therefore, we only have the 3 T’s as levers to change calorie consumption. These are Timing (of when to eat), Type (of food we eat) and Tracking (of calories we eat). Lastly, understand that by doing our digestion for us, a processed food ensures all of our calories are absorbed with maximum efficiency (which is bad).
So I can lose weight just by eating less calories? That's so NEAT! (Tracking)
To accurately know how many calories you need to eat daily to maintain or lose weight, you can enter it into any Total Daily Energy Expenditure (TDEE) calculator. However, we are terrible at estimating how many calories we eat daily (usually by under-estimating the amount). Studies show as high as 47% caloric under-estimation (and >50% exercise over-estimation)!58 Additionally, the FDA allows for 20% inaccuracy on the nutrition labels. Furthermore, we are poor judges of portion size as well (do not even look at the portion size of peanut butter). Of course it is possible to lose weight counting calories, however given inaccuracies with estimation it is very difficult (unless you eat certain types of foods, see below).
However, in a Cochrane Review (highest level of evidence in medicine) reducing portion size and/or using smaller tableware (plates, bowls etc), consistently decreased volume of food consumed by 22-29% (resulting in 200-400 fewer kcal/day)!65 High contrast plate colors, smaller serving utensils, keeping serving dishes off the table, pre portioning food, hiding or covering high-calorie food wrappers, eating more slowly, screen avoidance while eating, front loading water/veggies/soups also had effects.
Once we actually start to lose weight our body subconsciously (ie. not in our control) begins to slow down in a process called adaptive thermogenesis by regulating Non-Exercise Activity Thermogenesis (NEAT). Regular, small movements, such as walking, fidgeting etc make up the vast majority of calorie expenditure beyond our basal metabolic rate (BMR). Note that our metabolism does not change significantly as we age. It is the change in NEAT that accounts for up to 800 kcal a day in expenditure59. NEAT will also go down if you exercise that day. Observe your child’s movements to see how much more they move than you, even when sitting still #trying. This is the difference in NEAT and why it appears adults have a slower metabolism over time.
As this is subconscious, you will have to make a conscious decision to move more; bring on the exercise snacks! Exercise snacks are brief bouts of physical activity interspersed throughout the day. These can be climbing stairs, body weight exercises for a minute or a high intensity exercise for 20-30 seconds a few times a day. These snacks resulted in reductions in blood pressure equivalent to one medication, improvement in VO2max of 12% (see exercise section for why this is a big deal), and improved glycemic control66-68. Furthermore, treadmill desks, taking multiple brief walks per day, or even standing have been shown to be very beneficial. This is the main lever to pull on to increase your metabolic rate and calorie consumption.
To eat or not to eat (breakfast), that is the question! (Timing)
Time restricted eating (TRE) (AKA Intermittent Fasting (IF) for the purpose of this book) is one option to maintain a healthy weight and has numerous beneficial cardiovascular effects including decreases in weight, body fat percentage, hypertension, cholesterol and blood glucose20. TRE works by creating a calorie deficit essentially, in that a person is unable to eat more calories in a smaller window of time. In TRE/IF, a feeding window of 8, 10 or 12 hours is created where all calories are consumed regardless of source. The most studied is an 8-hour eating window with a 16-hour fasting window. Water, black coffee and/or tea (without any additions) appear to not break a fast. The clock starts when first consumption of calories is taken in. Note in the sleep section we are recommending stopping the last consumption of calories 3 hours prior to sleep. Note no significant differences have been observed in hypoglycemia/adverse events in diabetic patients, and the opposite is true, that lower A1c and improved glucose management has been observed.
Conversely, a first meal that is high in protein (a minimum of 40 grams of protein and unprocessed) has also shown reductions in overall calories throughout the day in certain studies and increased activity levels in the morning.51
Therefore, we recommend intermittent fasting to most people. The first meal and last of the day should be high in protein. The one group where we do not recommend intermittent fasting is young women (premenopausal). In this group the benefits of eating a protein meal in the morning align more with the circadian cortisol levels. This is especially true in women who are pregnant or who are experiencing missed periods.
But what about low carb, high fat, low fat etc diets? (Type)
In Keto 1.0, patients were able to lose weight because there were no processed foods that contained zero carbohydrates (note there is no “essential” carbohydrate). Now in Keto 2.0 there are keto cookies, ice cream, pizza etc. and people are gaining weight back the same as before. The Tsimane tribe in South America are an uncontacted tribe that have no known heart disease and are considered to have the healthiest hearts in the world22. They eat a diet that is 65-70% carbohydrates composed of white rice, yuka, chocolate etc. They violate every major macro diet (e.g. low carb) and yet have no heart disease. It is not about the macros. Autopsy data from Alaskan Inuit in the 1950’s showed less than one fifth the cardiovascular disease of the general population at the time (which was already much lower than it is today)23. Their diet consisted mainly of protein and fat. The macros do not matter (much).
No, I definitely heard that sugar is bad for you.
The following are all names of added sugar: {blank} sugar, {blank} syrup, Molasses, Nectar, Malt, Honey, {blank} concentrate, {blank}-ose, inverted {blank}, evaporated {blank}, {blank} juice, maldextrin, panela, agave, muscovado, panocha, sorghum, sucanat, and treacle. {blank} in this case could be any name followed by the word sugar/syrup or ends in -ose etc. Ingredients are listed first to last in terms of prevalence, however companies can list several names for sugar that when added up are the most prevalent. The AHA daily maximum for added sugar is no more than 9 teaspoons (36 grams, 150 calories) for men and 6 teaspoons (25 grams or 100 calories) for women and children 2-18 years old per day56. For children under 2 it is to be avoided. Note the authors of this book recommend zero added sugar to children under the age of 18. Sugar is addictive, full stop. It causes caloric overconsumption, insulin resistance, adipose accumulation, inflammation and lipogenesis (fructose specific fat creation in liver). Added sugars, preferentially become small dense LDL and TG in the body, leading to plaque formation in the arteries of the body. The reason to state it is not about macros is that added sugar only exists in highly processed foods (see appendix for food list). Conversely, ultra processed foods can now be made without added sugar and are just as bad (eg keto cookies). We always look for added sugars, but in the context of the overall processing of food. Fruits, while containing sugar such as fructose, also are very high in fiber, and therefore risk is mitigated compared to processed foods.
But what about protein?
Protein is broken down into amino acids which are the building blocks for structures such as enzymes in our bodies. As such they typically do not contribute to our overall energy balance. Protein is very satiating however, causing the GI tract to release PYY and GLP-1 which curbs appetite via the hypothalamus in the brain (like how GLP-1 injections work).
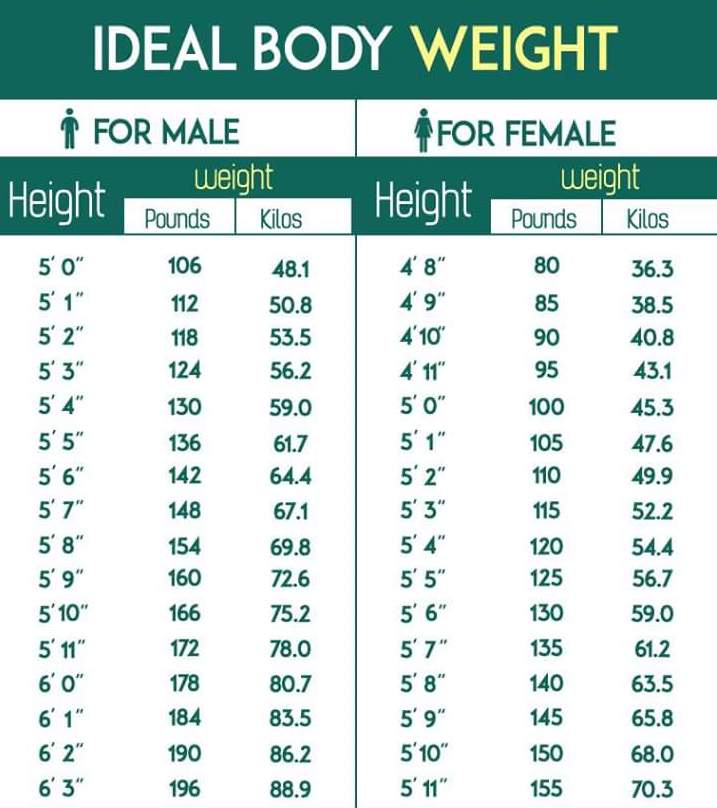
HOWEVER, the recommended daily allowance (RDA) for protein is only 0.8 grams/kilogram (a kilogram is 2.2 pounds)24. This is to prevent starvation and is entirely too low for optimal health. As such we recommend (unless you have significant kidney disease) approximately 1 gram of protein per pound of ideal body weight (see chart below for ideal body weight). Note: this is protein from actual food, quality makes a difference. The highest quality protein sources are from animals as they are the most varied, are the best absorbed, and contain the highest concentration of essential (essential = our bodies can not make them on our own) amino acids. Of the essential amino acids, leucine is the most important for building muscle. Also note you can build muscle just by eating protein, and that the ability of muscle to incorporate protein declines over time (likely from inactivity and not from intrinsic aging)25.
It is important to look at 24 hour protein intake over particular meals and timing, although muscles can only absorb about 25-30 grams of amino acids per meal. If protein comes from a meal, it gets absorbed in roughly 3-4 hours, whereas an animal protein shake can be absorbed in 30 minutes. Therefore, eating high protein meals for your first and last meal (for satiation), and overshooting the muscle absorption rate (eg. eating 40 grams of protein) is best. Note it is not as important to eat protein immediately after a workout, and is more important to focus on overall daily protein intake. Lastly note the evidence for protein intake cut offs/timing/quality is weak at best and further research is desperately needed in this area.
Ideal body weight for male and female by height. Note there is a +/-5 lbs margin of error and this is an approximation57
What about cookies, pizza, ice cream etc?
One can enjoy an occasional "treat" such as a cookie, pizza or ice cream. Consuming a diet that contains a large percentage of "unprocessed" foods but allowing small amounts of "processed" foods is acceptable and can be part of a healthy lifestyle. These food are highly palatable and enjoyable for a reason! It is a matter of balance. Bear in mind that it does take planning and effort to achieve this balance, particularly understanding the high prevalence of processed food that we encounter routinely in the grocery aisle and at most restaurants.
What about fast food/restaurants?
The vast majority of fast food and restaurant food is processed food. For example, in Europe, the bread in American style fast food restaurants is actually listed as cake (!) and multiple chains were caught using mattress chemicals in their breads (azodicarbonamide)26. In a number of states, the restaurants can be worse, as the fast food industry has to publish their nutritional information (although nothing about how they process the food which is the whole point). The impact of public-school nutrition on our children is significant, potentially contributing to the epidemic of childhood obesity. More importantly we are missing the opportunity to provide a solid foundation to our children for good nutritional habits for them to build upon as they mature. We recommend avoiding fast food/restaurants where possible, however we understand that socializing occurs frequently in these locations; which is a good thing (see social/misc section)! Therefore, to limit the damage, we recommend consuming a small high protein/fat meal e.g. a bowl of greek yogurt prior to the meal. That way you can order whatever you would like and just eat less of it.
What about specific diets? Mediterranean, DASH, Carnivore, KETO, WW, Flexitarian, Ornish, Paleo, Carnivore etc.
The Mediterranean diet (Med diet) is high in fruits, vegetables, whole grains, legumes, nuts, olive oil and moderate fish and poultry (as well as moderate wine intake). It has consistently shown improvement in lipid profiles and cardiovascular function while simultaneously leading to reductions in inflammation, heart attacks and strokes, resulting in a 23% reduction in all-cause mortality and 30% in cardiovascular risk62. We believe that the underlying principles for this are unprocessed food, high fiber, high omega and unsaturated fat content, as well as other nutrients. This diet is the most recommended framework because of its robust evidence and flexibility. Variations of this diet such as the MIND diet have shown similar results (although limited long-term data at this time for MED diet variations). This is the diet we recommend for most patients as a framework for optimal nutrition.
The DASH diet (Dietary Approaches to Stop Hypertension, see hypertension section) is the same as the Med diet, except emphasis is on low sodium/fat, no mention of alcohol use, as well as focus on lean protein sources (not necessarily fish focused). Indeed, the DASH diet was shown to be superior to the Mediterranean for blood pressure control. Mediterranean was shown to be superior to DASH for long term CV health, diabetes prevention, weight loss and cognitive function63. This is the diet we recommend if high blood pressure is your main CVD issue.
The flexitarian diet is primarily plant based with occasional meat/fish. While this diet follows the principles of this book, there are less rules/long term follow-up studies. The old med school nutrition adage of “eat small, mostly plants” seems to sum up the flexitarian diet nicely. It is difficult to find long term CVD studies as by definition flexible is part of the flexitarian diet.
WeightWatchers (WW) - now with or without GLP1 support, uses a point based system for the content of foods. It emphasizes accountability with check ins and offers flexible food choices, however it is costly (as a membership fee) and maybe cumbersome secondary to consistent food logging. Long term CVD outcomes studies are limited.
Ornish Diet – very low fat, mainly vegetarian, allows from some nonfat dairy and egg whites. It is difficult to maintain fat intake of 10%. Very low fat diet can regress atherosclerotic plaque in 1-5 years (but small patient numbered studies)64.
Volumetrics Diet – focus on low energy dense foods such as soups to improve satiety and weight control. This diet may support weight loss and improved inflammation levels, meal prep maybe a problem and it does miss incorporation of healthy fats seen in the Med diet. No long term CVD studies are available at this time.
Glycemic Index (GI) Diets – South Beach Diet etc. Glycemic index refers to individual foods’ effects on blood sugar (in relationship to sugar itself which has a GI of 100. A low GI food would raise blood glucose to <55 while high one would raise it >70. For example eggs have a GI of 0 while Pineapple is 74. This has not translated into CVD outcomes in long term studies, secondary to macronutrients, lifestyles, calorie intake etc, appearing to play larger roles.
Low Carb Diet (Atkins, Keto) diet – high fat, moderate protein and very low carbs. This diet leads to rapid weight loss, however now there are keto cookies, etc. which have shown to promote weight gain regardless of macro intake. This is an interventionist diet and it works well initially. We use this diet up front to induce rapid weight loss and to correct metabolic issues. However, this diet is unlikely to be sustainable long term given the dietary restriction, and very few, if any, patients stay on it in the medium to long term. Therefore, for diets like keto, paleo and carnivore, initial use it upfront, with plan to gradually switch to MED diet long term. Note fiber also lacking.
Paleo diet - focuses on foods that were around in the Paleolithic era. This diet follows unprocessed food, but does completely eliminate dairy/grains, leading to possibly overly restrictive as well. No evidence for CVD long term outcomes. As above, is an interventionist diet. Note fiber also lacking.
Carnivore diet – exclusively animal products. Much like Keto, LDL/ApoB can go extremely high, which is a risk for CVD over the long term. No long term CVD outcomes trials. As above, is an interventionist diet. Note fiber also lacking.
What about snacking?
Across the board, the results have been mixed on snacking. While the NHANES III study showed some benefit to increased meal frequency, Chapelot et al showed that snacking usually resulted in a positive energy balance (and therefore weight gain)52. Given these mixed results, we recommend self experimentation here to see if snacking benefits you. Choosing high protein, unprocessed food snacks is likely the most beneficial if you do decide to snack.
What about saturated fat intake?
Saturated fat is found in animal and dairy products and some plant products such as coconuts and palm oils. Once ingested they can go to the liver and raise the LDL cholesterol (see cholesterol chapter). Some studies suggest insulin resistance as well27. The mechanism of insulin resistance may be related to lipid intermediates that accumulate in muscle cells (the main regulator and storage of sugars) leading to insulin resistance. However, two very well-done studies in the 1970’s (the Minnesota Coronary Experiment28 and the Sydney Diet Heart Study29) showed that replacing saturated fat with polyunsaturated fat (i.e. vegetable oil/linoleic acid) led to higher mortality. For every 1% increase in energy from polyunsaturated fats there was a 17% increase in death. Overall, at this time, we feel context matters, and the recommendation is to not limit or follow saturated vs. unsaturated fats, but instead to focus on high quality, unprocessed foods as above. Additionally, saturated fat raises large buoyant particle size LDL, not small particle size LDL, and therefore has significantly less effect on artery plaque formation.
*** Caveat: Approximately 1 out of 250 of you reading this have Familial Hyperlipidemia (FH) [see cholesterol section]30. The treatment for this is a low saturated fat diet! The mechanism is likely related to over stimulation of lipids, specifically LDL in FH, which is exacerbated by saturated fat. Get your ApoB tested!
What about Alcohol?
One Beer (12 0z) = 1 glass of wine (5 oz) = 1 shot of distilled alcohol (1.5 oz). One standard drink is 14 grams of Ethanol. There is no safe level of alcohol consumption for the heart31. It leads to cardiovascular disease, hypertension, strokes, arrhythmias and addiction. It is calorie dense and leads to weight gain secondary to alteration in the hormones that regulate hunger and satiety (ghrelin and leptin). Alcohol causes inflammation, reactive oxygen species (aka free radicals), neurocognitive deficits and leaky gut/inflammation. There have been studies showing the benefits of moderate consumption of alcohol, particularly red wine. This recommendation is found in the Mediterranean diet and in the French paradox, where it is observed that French citizens live longer than Americans despite high levels of smoking and saturated fat (although see above)32. It is thought to be secondary to red wine consumption which contains resveratrol, however you would need to drink around 400 liters of red wine a day to get 1 gram of resveratrol (note we do not endorse resveratrol either). When broken down by region, the higher red wine consumers in France also ate more fruits and vegetables, negating the effects of red wine itself. An alternative explanation to the French Paradox is less processed food eating overall (healthier) and a more social component to alcohol use. Again, like processed foods, sugar etc. the dose makes the poison. Overall, we follow the Canadian guidelines of 2 standard drinks maximum per week33. What’s the point you ask? Indeed.
What about water?
Adequate water intake can lead to weight loss, lower risk of metabolic syndrome and even a lower risk of fatal coronary events70. Having water prior to a salty meal can balance out the effects of that sodium load (see hypertension section). Recommendations for the amount of water that should be consumed on a daily basis vary, however, a general rule is to aim for drinking enough water to have pale yellow urine and aim for one liter of water extra per hour of exercise. Do not consume water from plastic bottles (see microplastic section).
What about artificial sweeteners?
Artificial sweeteners potentially lead to weight gain by activating the pancreas and digestive system via sweet receptors in the tongue34. When no calories are detected, these organ systems send signals to the brain to seek out calories rather than shut down. Additionally, they affect the gut microbiome (see below) in ways that we do not understand35. Some appear safe such as Xylitol which may block Strep Mutans proliferation in the oral cavity (the bacteria that causes cavities) while others such as Aspartame are now being labeled as a potential carcinogen36,37. The research is evolving in this area and at this time we cannot recommend use of artificial sweeteners.
What about fiber?
Fiber has a complex architecture, which is why you cannot process fiber and put it into food. There are two types of fiber, soluble and insoluble. Soluble fiber forms a gel and coats the digestive tract. It comes from whole wheat (not processed), fruits such as apples and vegetables such as carrots (you can search up a more exhaustive list). Insoluble fiber forms a scaffold and adds bulk to stool, preventing constipation and comes from beans, nuts and seeds. These two sources of fiber interact with our gut microbiome (see below) to lead to weight loss, reduced calorie absorption (through coating the intestines) and improved insulin sensitivity.
Fiber is a main prebiotic (see below) which allows bacteria to ferment and produce short chain fatty acids (SCFAs) which have many beneficial effects such as reduced inflammation (inflammation is a precursor to cardiovascular disease), metabolism satiety (interaction with L cells of intestine to create GLP-1, see below), and maintaining gut barrier integrity38. Some individuals experience gastrointestinal discomfort or bloating from excess fiber ingestion, which can be severe. We recommend gradually increasing your fiber intake (of both kinds and from natural sources) until you begin to feel GI discomfort and then lower the dose to the maximally tolerated (aim for 25-35 grams per day, but you must be able to tolerate it!)39.
Why can’t you just tell me what to eat? Tell me the superfoods to consume!
Nutrition science has several fundamental challenges that make it difficult to draw conclusions and to apply them uniformly to an individual. First, data is usually in the form of self-reported diet surveys, which are prone to errors such as recall bias, underreporting and misclassifications of foods. Second, confounding factors like genetics, cooking style, individual characteristics like gut microbiome, socioeconomic status, different macronutrients within the same food and quality of food in the same category. This is why the nutrition papers that make the news are rarely relevant to the individual patient, and we would not recommend making dietary/lifestyle changes based on those papers alone.
What about probiotics?
Probiotics are living beneficial (aka good) microbes, prebiotics are food for these microbes eg. fermented foods [Kimchi, pickled foods] and fiber (see above), and post biotics are the beneficial compounds produced by these probiotics. Most probiotics purchased in supplement form (on shelves, not refrigerated, not in food) are DOA (dead on arrival)40. There are a few companies that are at least proven to be alive on arrival (look for ones that come refrigerated and have actual studies). Moreover, since probiotics are considered a supplement there is no regulation on the type, quantity, dosing, or health outcomes associated with ingestion of these. Unprocessed Greek yogurt which contains these probiotics appears to be beneficial in appetite regulation, and even can lead to the reduction in the risk of type II diabetes41. In theory, certain species such as Akkermansia will interact with L cells of the intestines to tell the pancreas to release GLP-1, while simultaneously altering the absorption of various nutrients (see below)42. Furthermore, we know transplanting the microbiome from an obese to a thin mouse can cause the thin mouse to become obese43. The gut microbiome can also affect inflammation through lipopolysaccharide production (which is bad) and reactive oxygen species scavenging (a common pathway with atheroma aka plaque formation in the arteries). We believe this (and above, see fiber section) are the reason why fiber has been proven to have beneficial cardiovascular outcomes. More research is needed in this area before recommendations on specific probiotics can be made, although the literature looks promising and will be an area of future advancement in the field of preventive cardiology.
What about organic vs. non organic foods?
Organic food is defined as food produced without the use of toxic and synthetic pesticides and fertilizers, genetic engineering, antibiotics, synthetic growth hormones, artificial flavors, colors, preservatives, sewage sludge and irradiation, according to the USDA website. Furthermore, pesticides on non organic food contain endocrine disruptors, obesogens and other toxic chemicals. While eating organic intellectually makes sense from a cardiovascular standpoint, the studies have not shown improved outcomes at this time. Likely, this is because people who buy organic food also have other traits that lead to good health, such as regular exercise. Therefore, our recommendation is it is probably smart to buy organic if you can afford it, however it is not a must, and is much better to buy unprocessed food than to buy processed.
Should I own a scale?
Regular use of a scale to measure weight (although now scales can even estimate body fat percentage etc) has led to increased weight loss and improved BMI53. We recommend weighing yourself daily (in the studies even 3x/week led to worse results). This will help guide you on your journey to improved CV health and will allow you to see any changes that may need to be made.
Should I write down what I am eating?
A short-term food journal of approximately 2 weeks can impact dietary choices, body weight and associated CVD risk factors. This was largely due to awareness of what participants were actually eating in terms of calorie count, processing of foods, and portion sizes. Participants who food journaled lead to greater impacts in weight loss, cholesterol levels and blood pressure than those who did not. We suggest starting a food journal when you decide to follow the advice in this book, to monitor for hidden habits that maybe impeding your journey to CVD health.60
What are those discs on peoples’ arms? What is a continuous glucose monitor? Should I get one?
Continuous glucose monitors (CGMs) painlessly attach to the arm and provide 24/7 monitoring of glucose. Most studies however have focused on short to intermediate term endpoints such as HbA1c or time-in-range improvements rather than hard cardiovascular endpoints. However, observational data would suggest that sustained improvements in glycemic control over time may translate into reduced CVD risk. A case in point is adding protein to carbohydrates may blunt the immediate postprandial (post meal) glucose spike but can prolong the glycemic excursion, leading to unclear benefit over time.61 Walking (just 10-15 min) after eating however has been shown to reduced postprandial (post meal) glucose (blood sugar) and triglyceride spikes, and is a recommended and excellent way to decrease these parameters post meals69.
How do I lose those last 5-10 pounds?
It is important to note that there is not a single “goal weight” for everyone. Aiming for a body mass index (BMI) of 19-25 kg/m2 serves as a very rough guide. We generally couple this with bloodwork and body composition scans to ensure that you are metabolically healthy. Once you are approaching your goal weight it is much more important to focus on body composition than what the scale says.68 This translates into increasing your lean muscle mass, maximizing your cardiorespiratory fitness and improving your fat distribution (Hint: you are already doing this by reading this book!)
What about Atrial Fibrillation?
Atrial fibrillation is the most common arrhythmia in the world and approximately 25% of all strokes come from atrial fibrillation!!!! As of 12/2023 the atrial fibrillation guidelines have listed weight loss as a class 1 (highest level) of recommendation for any patient with a BMI > 27 kg/m2) with an ideal target of 10% weight loss44.
What about pharmacotherapy for obesity?
Over the past few years there has been an explosion in the use of pharmacotherapy for obesity. The two most commonly prescribed medications currently are Ozempic (for diabetics) = Wegovy (for non-diabetics) = Semaglutide [they are the same molecule]45 and Mounjaro (for diabetics) = Zepbound (for non-diabetics) = Tirzepetide [they are the same molecule]46. Semaglutide is a full agonist (meaning full activator) of glucagon-like peptide -1 (GLP-1) in the pancreas whereas Tirzepetide is a partial agonist of both GLP-1 and GIP. There are going to be several variations of these medications coming on the market (the next generation will add glucagon to increase the basal metabolic rate) but for now we will focus on these two. The basic mechanism of these medications is to slow the digestion of food motility aka slow the speed of food going through the digestive tract and interact in the brain to decrease hunger in ways that are poorly understood47. Note that they do not bind sugars. Note also that if GLP-1 agonists slow gut motility and lead to weight loss, then the opposite must be true, that foods that speed through the digestive tract i.e. processed foods must lead to weight gain.
These medications have extensive benefits in terms of cardiovascular outcomes, including decreases in weight, insulin resistance, HbA1c, blood sugar, hypertension, cholesterol levels and secondary cardiac outcomes such as prevention of heart attacks, atherosclerosis and strokes. Secondly, the 4th leading cause of death in America is medication interactions, and because of the improvements in the above, it allows patients to come off of other medications. Thirty six percent of patients in the USA take > 5 medications, and the odds of a drug-drug interaction are 100% at 8 medications48.
However, there are several significant downsides to these medications including cost ($1400/month in some cases!), supply issues, gastrointestinal side effects (at 10-16% range, nausea and constipation most common), gastroparesis (paralysis of the stomach motility which is reversible), bacterial overgrowth syndrome, weight gain upon discontinuation (see below for mitigation protocol), medication interactions (poorly understood), decreased fluid intake (maybe beneficial in case of alcohol abuse), pancreatitis, medullary thyroid carcinoma, and dissociation (most serotonin is stored in gut, maybe related to the effectiveness of the medication?). Tolerance may develop leading to higher dosing requirements. Furthermore, they may also lead to worsening sarcopenia (muscle loss, which we consider the most serious common side effect) where these medications cause equal loss of fat, bone, muscle and connective tissue. Note, muscle quality (and not just muscle mass) is very important for metabolic regulation (see metabolic section) and these medications do nothing to improve that quality (in addition to lowering the mass).
Often, patients are either too debilitated or too addicted to processed foods/alcohol to begin to exercise and diet seriously. Furthermore, studies back fast initial weight loss in terms of greater weight reduction and long-term maintenance, and patients who utilize fast weight loss protocols are not more susceptible to weight regain than more gradual weight loss49. In other words, casinos are popular for a reason!
We begin by determining if a patient is appropriate for pharmacotherapy (you must check with your doctor). It is important to offer a non-pharmacotherapy option as well, so a patient can decide. We typically utilize BMI >27 kg/m2 and one cardiac risk factor such as hypertension or diabetes (in addition to other patient characteristics on an individualized basis). There are also multiple drug interactions and caveats that you and your physician must discuss before initiating.
Our protocol is individualized and is based on the following: early introduction of weightlifting/resistance training, frequent follow ups for titration and side effect assessment, teaching the tools in this book to change lifestyle and behavior (including processed food elimination, TRE, sleep and foundational exercise introduction), followed by a gradual off titration or steady state dosing. We utilize DEXA scanning and regular bloodwork to follow muscle mass, visceral fat quantification and multiple other parameters at specified intervals to avoid sarcopenia and other risks/medication interactions. We have seen success in this manner with patients maintaining profound weight losses over more than 18 months.
It is important to note that at this time, the long-term outcomes/side effects of these medications are unknown. It will take many years to understand the full effects of these medications, while newer and different peptide agents will be coming out in the market which may have different properties. You must work with a health care provider who is knowledgeable about the risks and benefits of this class of medications, is willing and able to follow you closely, and have an individualized approach to care. We believe that this will ensure a safe approach to maximize the benefits of this class of medications while minimizing the long-term risks, and at the same time introducing the core principles of preventive cardiology to the patient.
Key Points: Obesity-Metabolic Dysfunction and Nutrition
Metabolic dysfunction is the root cause of most cardiovascular diseases by driving inflammation. It is caused by a combination of processed foods and lack of exercise. Most importantly, it is curable!
While excess calories is the cause of obesity, eating processed foods is what drives us to consume those excess calories.
Eating an unprocessed, high protein and fiber diet is extremely beneficial for health and longevity. For protein aim for 1 gram/pound of lean body weight and for fiber aim for approx 25 grams per day.
There is pharmacotherapy to treat obesity, however it is a double edged sword and you should follow your physician routinely when on these medications.