Sleep and Its Impact on Cardiovascular Health
By: Kyair Smith MD, Benjamin Ravaee MD, Jonathan Kahan MD
What you need to know
Sleep is part of the cornerstone of cardiovascular health. If you have poor sleep, it is very difficult to be healthy from a cardiovascular standpoint.
Medications, substances, and supplements rarely work for sleep and have side effects that destroy sleep architecture, diminishing the health benefits of sleep.
Today our sleep is worse than ever before. A lot of people struggle with sleep, it's ok! There are good techniques to help with sleep. If they don't work, a sleep expert is available as well.
Why do we need sleep?
Sleep is a necessary physiological process essential for overall health and well-being. Beyond its role in rest and restoration, emerging research has highlighted the intricate connections between sleep patterns and cardiovascular health. In this exploration, we delve into the multifaceted relationship between sleep and cardiovascular disease (CVD) while exploring the effects of sleep on cardiovascular fitness. The most important reason to sleep is this: sleep allows us to live our lives to the fullest potential and without adequate sleep, life cannot be enjoyable.
How does sleep work?
There are two main biological processes that regulate our sleep; the first one being circadian rhythm where the environment inputs onto our internal clock, and the second being sleep pressure regulated by adenosine levels. Our internal biological clock, also known as the suprachiasmatic nucleus (SCN), functions to coordinate our bodies' activity levels to the rising and setting of the sun using hormones and the autonomic nervous system. To generate and coordinate automatic processes such as heart rate, wakefulness, and hormone levels, the SCN requires repeated metabolic cues from environmental factors such as light exposure, sleep, activity, and feeding (circadian rhythm).1
On the other hand, adenosine and its receptors are postulated to play a role in sleep pressure and intensity. Adenosine buildup is a consequence of cellular metabolism and is produced from the breakdown of ATP, the main cellular energy source. Thus, the longer we are awake and active, the more adenosine accumulates in the areas of our brain related to arousal.2 The accumulation of adenosine translates to increased sleep pressure which allows you to fall asleep earlier and more deeply.
What are sleep stages?
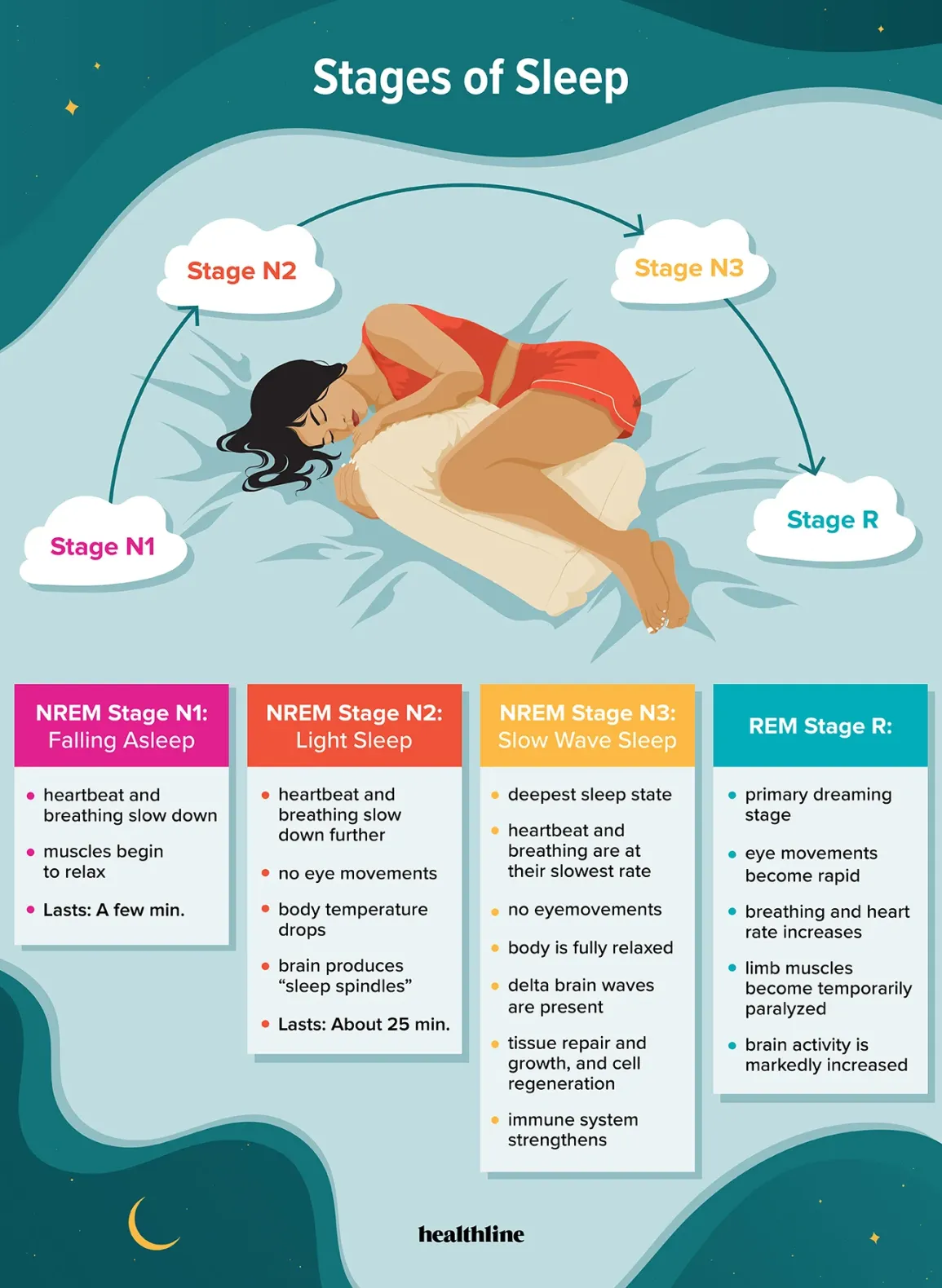
There are five stages of sleep: Awake, N1, N2, N3, and Rapid Eye Movement (REM). Approximately 75% of sleep is spent in the non-REM (NREM) stages (N1-N3), with the majority spent in the N2 stage. A typical night's sleep consists of 4 to 5 sleep cycles (each approximately 90-120 minutes long), with the progression of sleep stages in the following order: N1, N2, N3, N2, REM.
The N1 stage is the lightest form of sleep, it occurs during the first 1-5 minutes of falling asleep, and is the shortest phase of the sleep cycle. The N2 stage is a deeper sleep, characterized by specific brain waves known as sleep spindles and/or K complexes. These distinctive patterns are only found in N2 sleep and are thought to be caused by the intense neuronal firing that occurs during memory consolidation.3 Of note, you cannot control your sleep stages.
The N3 stage, also known as the slow wave stage, is the deepest form of sleep and is the time when rejuvenating processes such as tissue repair and regrowth, bone and muscle formation, and the immune system resets occur.
Last is the Rapid Eye Movement (REM) stage. During REM sleep, the body remains paralyzed, but the muscles of the eyes and the diaphragm are not, thus the characteristic rapid eye movement that can be observed. Interestingly, the amount of REM we experience decreases as we age, with infants having the highest levels of REM. Note for every 5% decrease in REM sleep there was a 13% increase in all-cause mortality in adults!36 This leads to the hypothesis that REM sleep plays an important role in memory consolidation, emotional development and motor learning.4
Figure 1. Stages of Sleep4
How does sleep chronotype affect sleep?
Sleep chronotypes are defined as an individuals' natural proclivity to sleep during a certain time of day5. Most experts agree on 2 major categories of sleep chronotypes- earlier or later chronotypes with some reports of intermediate types. The earlier chronotypes are what many would refer to as a “morning person” or “early bird”. These people prefer to wake up earlier, experience peak physical and mental activity closer to awakening, around 10am-noon, and go to sleep earlier as well. Conversely, the later chronotypes are characteristically known as “night owls,” persons who prefer to wake up later around 10-11am, peak activity around 3-6pm and fall asleep later in the night. If you are unsure which type you are, you can look up the MEQ test, which is a 20 question test that will tell you which chronotype you are.
When our sleeping habits are in misalignment with our internal biological time clock, this is referred to as circadian misalignment. If this misalignment is due to social obligations such as school, work, even entertainment purposes this is known as social jet lag (SJL) due to the difference in sleep patterns observed between working days and free days.6 Research has proven that our sleep chronotype may affect our sleep quality, with negative effects on sleep, such as increased difficulty falling asleep, more nighttime awakenings, greater caffeine consumption, and decreased amounts of REM sleep being more prominent in the night owl groups. Similarly, studies show that later chronotypes typically experience more social jet lag with the effects being insomnia, mood changes, fatigue, and difficulty concentrating; although, there have been no reported differences in objective measures of daytime alertness and cognitive functioning.6 Chronotype can therefore predict circadian disruption, and as such, affect sleep-wake cycles and potentially sleep quality.
The conclusion that evening chronotypes are more likely to have circadian misalignment and increased sleep debt gives us a clue as to why later chronotypes are associated with negative cardiovascular effects. More specifically, just one hour of SJL or sleep debt, which has been shown to be more prevalent in night owls, increases the risk of cardiovascular disease by 11%.5 Contributing to this point, one observational study showed that individuals who sleep later had higher body mass index (BMI), ate more calories after 8:00 PM, and had less healthy diets overall.7 In addition, individuals with a preference for later bedtimes were more likely to be obese, have diabetes and/or hypertension, further indicating the role sleep chronotypes may play in cardiovascular disease.7
With this in mind, those who identify as later chronotypes could make attempts to alter their chronotype in order to avoid the negative health effects associated with circadian misalignments, although this may be easier said than done. Since chronotype is mainly dependent on non-modifiable factors such as age, gender, genes, and geographical location, studies that attempted to alter chronotype have only been successful in changing the median sleep time for at most two hours by making changes in behavioral and environmental input.8 This can be done by setting your alarm 2 hours earlier, eating a high protein first meal, getting outside early (direct sunlight, no glass filter!) and exercising earlier, as well as going to bed earlier by 2-3 hours.
How much sleep should I get?
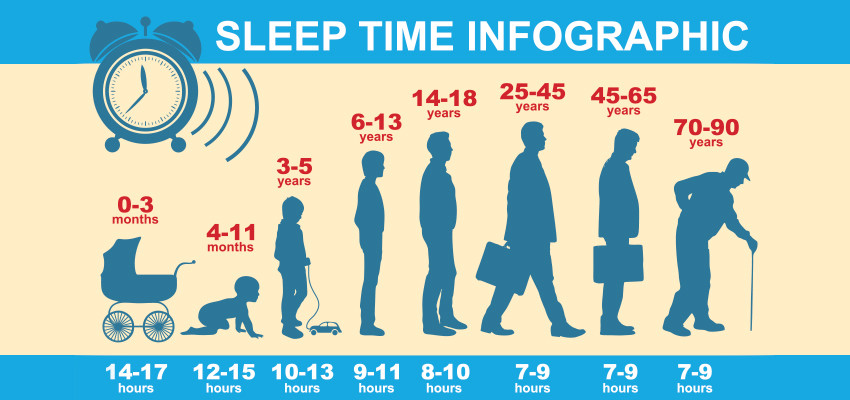
Figure 2. How much sleep do we need according to age9.
The duration of sleep plays a crucial role in cardiovascular health. The National Sleep Foundation recommends 8 hours of sleep a night to maintain optimal health in adults. Unfortunately, studies show that the average duration of sleep in Western societies has decreased from 9 hours in 1910 to less than 7 hours today.9 And even more concerning, people who do shift work, defined as any job that operates outside of the typical 8am-5pm (including parents of young children!), often report getting 5 hours of sleep or less. This is roughly 15 million Americans; including health care providers, factory workers, firefighters, bartenders, food service workers, and many more that fall into this category. Epidemiological studies have consistently demonstrated a U-shaped relationship between sleep duration and the incidence of coronary heart disease (CHD), with both short and long sleep durations associated with an increased risk.9
Short sleep durations, defined as less than five hours per night, have been linked to hypertension, atherosclerosis, and other cardiovascular conditions due to their detrimental effects on metabolic and inflammatory pathways.10 Sleeping less than 5 hours a night could lead to hypertension through elevated sympathetic nervous system activity, increased cortisol (the stress hormone), and increased catecholamines (fight or flight response), causing elevated blood pressure (BP) the next day.11,12
Similarly, chronic sleep deprivation leads to structural adaptations by the cardiovascular system to adjust to continued elevated BPs, such as thickening and remodeling of the heart which can also contribute to worsening cardiovascular function.13 This could also contribute to hypertension by disrupting circadian rhythmicity and autonomic balance by way of decreased metabolic activity due to altered sensory input. Furthermore, hypertensive subjects have been shown to have reductions of >50% in the 3 main neuronal populations of the SCN in comparison to normal subjects.10
Conversely, excessively long sleep durations may also add to cardiovascular risk through decreased physical activity, and a more sedentary lifestyle, suggesting the importance of achieving optimal sleep duration for cardiovascular health. You can catch up on sleep during the weekends to negate the effects of shorter sleep during the weekdays39. Additionally, you can “bank sleep”, where you sleep as much as possible where you can, leading up to a period where you know you will be sleeping less. Exercise has been shown to mitigate the effects of short sleep duration as well.
How Does Sleep Quality Impact Cardiovascular Health?
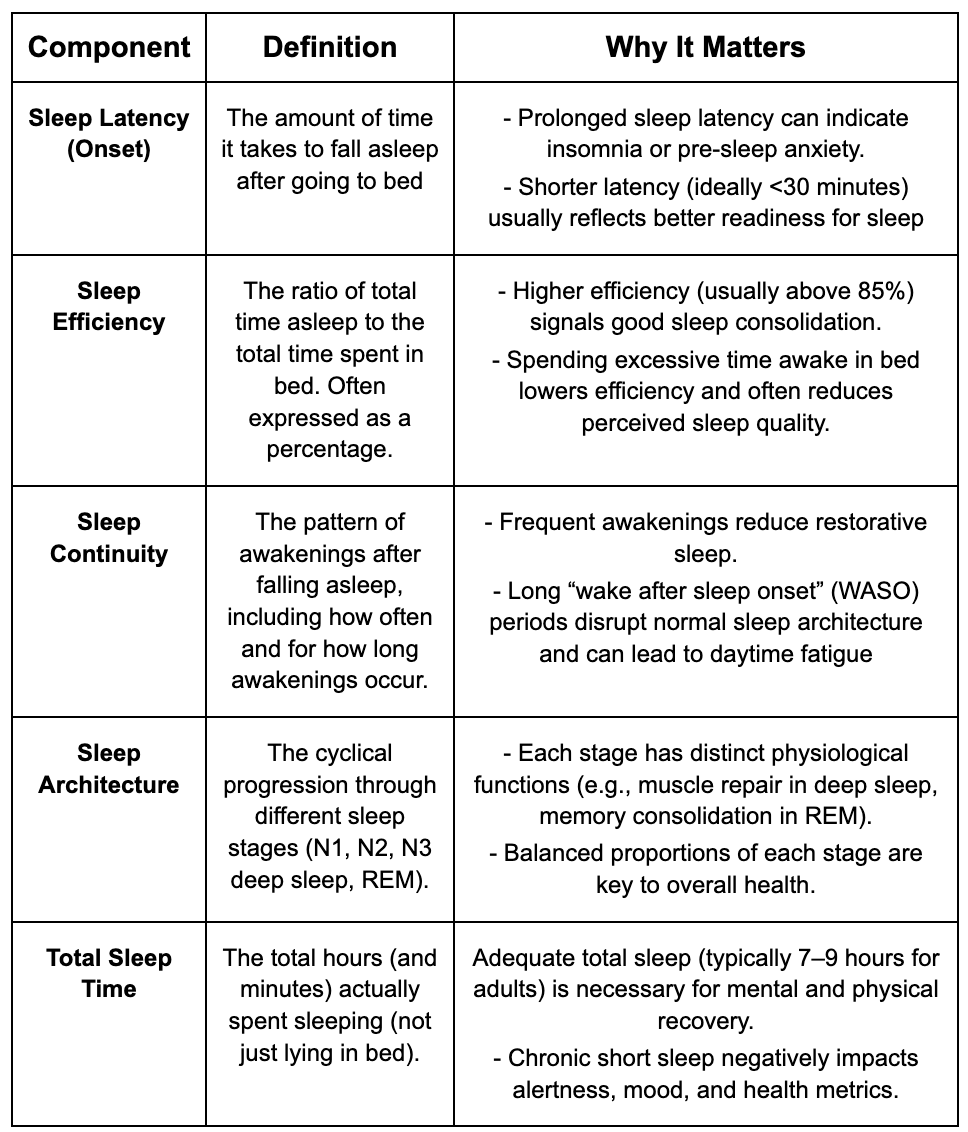
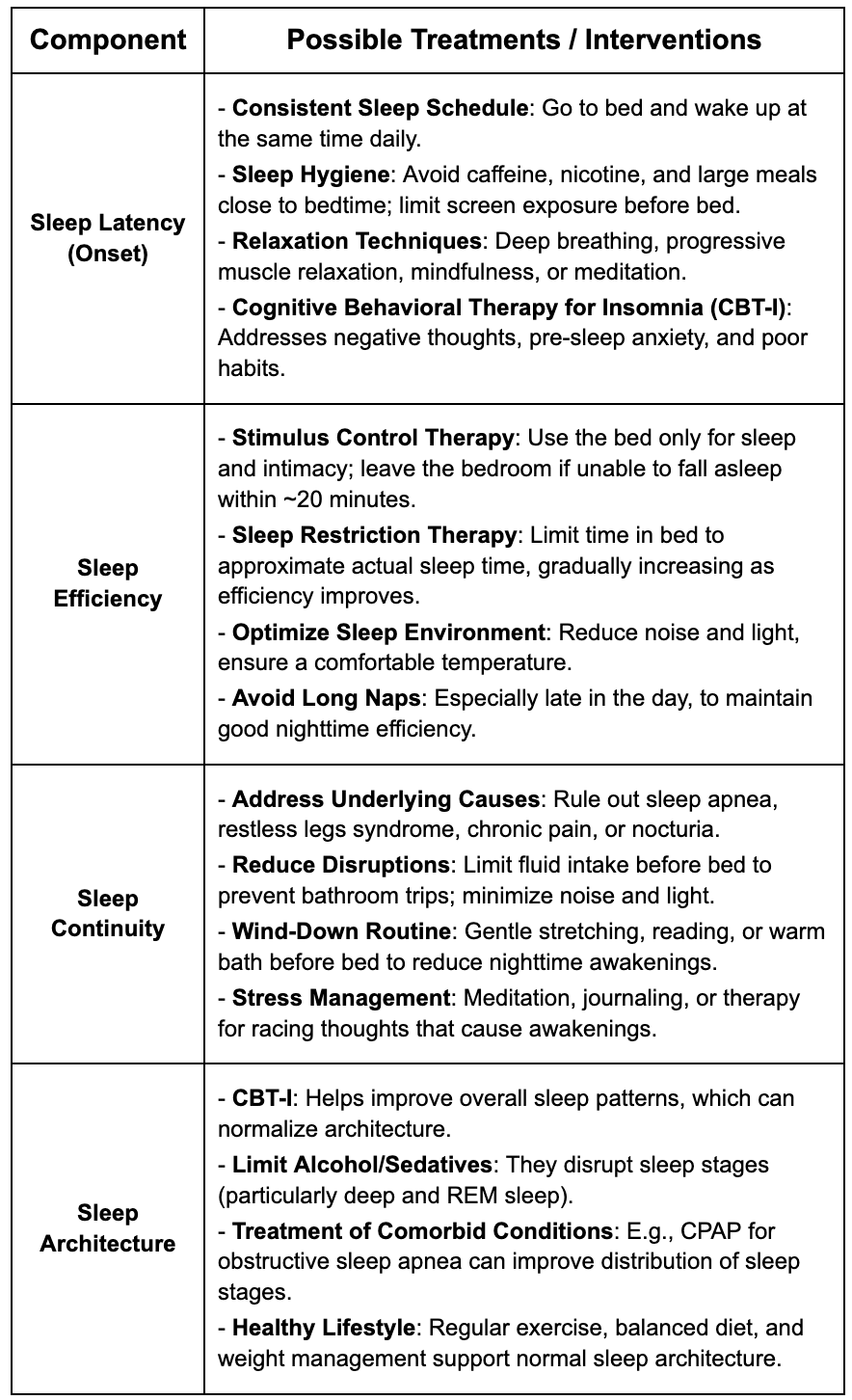
Sleep quality is broken down into components listed below, each of which can be manipulated to improve overall sleep: To check if you have a sleep quality issue, we recommend the Pittsburgh Sleep Quality Index (PSQI) calculator (find an online version that automatically calculates for you). The PSQI will tell you not only if you have a sleep quality issue but point you to which type you have.
The quality of sleep significantly influences cardiovascular outcomes. Poor sleep quality, characterized by frequent awakenings, disturbances in sleep architecture, and sleep disorders such as sleep apnea, contribute to the development and progression of cardiovascular disease. Additionally, studies have shown that acute sleep deprivation during the first part of the night causes the physiologic drop in blood pressure and heart rate to be blunted during the hours of sleep deprivation. This causes increased BP readings the following day which is supported by an increase in urinary excretion of norepinephrine and epinephrine observed during the sleep-deprivation night.12
Elevated plasma concentrations of C-reactive protein (CRP) are indicative of systemic (chronic) inflammation and are used as a marker for cardiovascular health and fitness. In a study conducted by Meier-Ewert et al. where they measured levels of high-sensitivity C-reactive protein (hs-CRP) in healthy adults who stayed awake for 88 continuous hours; the hs-CRP concentrations and systolic BP increased during the period of sleep deprivation, which further demonstrates a relationship with sleep deprivation and cardiovascular inflammation.14
What are the treatments for specific sleep quality issues?
Which is more important, sleep quality or sleep regularity?
Sleep regularity (going to bed and waking up at the same time) has been shown to be a stronger predictor of all-cause mortality and cardiovascular outcomes than quality!40 We have fixed schedules and wake up times are usually not flexible (school, work etc). However, our variation of going to bed can vary drastically. Regularity is defined as bed/awakening times within 20 minutes of each other. Setting a regular bed/wake time is one of the best things you can do for your health!
How does obstructive sleep apnea affect sleep?
Obstructive sleep apnea (OSA), in particular, is associated with increased sympathetic nervous system activity, oxidative stress, and endothelial dysfunction, all of which promote cardiovascular pathology and increase the risk of adverse cardiovascular events.15,16 These changes may be related to patients’ lifestyle, meaning the daytime somnolence caused by sleep apnea may predispose individuals to a lack of physical activity, to consume more calories and consequently gain weight. The increase in weight, more specifically increased deposition of fat in the upper respiratory system causes further narrowing of the airways which worsens the sleep apnea, causing a vicious cycle.17,18
How do I diagnose and treat sleep apnea?
Initial questionaries such as STOP-BANG can accurately diagnose sleep apnea risk. If you do not know if you snore you can download the free app SnoreLab® which will record your sleep to see if you snore. From there, a sleep study (either at a sleep center or home sleep evaluation) can be obtained which can formally diagnose you. Treatment focuses on weight loss, including the use of GLP-1 agonists, as well as devices that your sleep medicine physician can guide you on. Gone are the days of the standard CPAP mask as the only solution for OSA and we recommend anyone with an elevated score of 2 or more on the STOP-BANG questionnaire to begin working with a sleep medicine physician to formally diagnose and begin to treat this systemic condition. Do not under-estimate how much sleep apnea can affect your life.
How does caffeine affect sleep?
Coffee/Caffeine has been shown to have beneficial health effects, such as reducing the risk for some types of cancer, decreasing the chances of developing diabetes, and lowering the risk for heart disease and stroke. Research shows that these benefits of coffee are attributable to both the caffeine and antioxidant/anti-inflammatory properties. Note coffee specifically is America’s main way of obtaining antioxidants and over 90% of people worldwide are coffee drinkers20. Caffeine has persistently shown to lower the risk of type 2 diabetes (antioxidant effect), as well as improved lipid profiles and cardiovascular health.20
Caffeine is an adenosine-receptor blocker, it functions to oppose the sleep pressure properties of adenosine. Therefore, caffeine causes increased alertness and arousal by blocking the natural effects of adenosine and delaying sleep homeostasis and decreasing sleep pressure.2 Caffeine is found in a number of foods and beverages, such as coffee, tea, dark chocolate, medications and energy drinks, with an average cup of coffee containing around 95 milligrams of caffeine.20 Decaffeinated coffee, produced by extracting caffeine from coffee beans, contains significantly less caffeine, typically ranging from 2 to 5 milligrams per 8-ounce cup but delivers the same aroma and flavor as a regular cup of coffee.
It is important to note that there are several ways to decaffeinate coffee, with the water or carbon dioxide methods being the safest. The effects of caffeine can usually be felt within 30 minutes of consumption; however, the effects can last anywhere from 2-10 hours depending on tolerance (The half (T½) life of caffeine is 5-6 hours, the quarter (T¼) life is 10-12 hours), metabolism and genetic factors (highly variable CYP450/AHR gene clearance which we can test for). That means that if you drink coffee in the afternoon, you may still have caffeine present in your system at night!
We recommend no caffeine after 11 am at the latest because of this. Caffeine in the afternoon/evening can lead to sleep fragmentation, especially stage 3-4 sleep and blunting of N1 sleep. Habitual use can lead to upregulated adenosine receptors in the brain, leading to tolerance. Taking occasional caffeine breaks can help mitigate this. Of note energy drinks are not safe, as they contain very high levels of caffeine (in addition to sugars and other harmful additives) and can be consumed very quickly (why the army has banned their use as it can lead to arrhythmias which may be fatal).
How does alcohol affect sleep?
Although many report using alcohol to help fall asleep (due to its sedative effects), the metabolites of alcohol can significantly disrupt sleep throughout the night as they are continuously metabolized in the liver. A standard drink contains approximately 14 grams of ethanol. This will reach peak blood levels in about an hour, but it will take approximately 25 hours to be cleared from the body entirely. However, the effects of alcohol depend on the amount consumed, the rate of metabolism, the speed of consumption, BMI, gender and several other factors. Alcohol increases N3 sleep at the beginning of the night, but it suppresses REM sleep, which causes significant sleep fragmentation and awakenings during the latter half of the night, leading to overall nonrestorative sleep.21 Additionally, chronic alcohol consumption and/or alcohol use disorder has been shown to disrupt the circadian rhythm and sleep homeostasis, leading to worsened symptoms of sleep apnea, insomnia and vivid dreams.21 These effects can lead to worsened withdrawal symptoms and increased chances of relapse in those with alcohol dependence.
How does nicotine affect sleep?
Smoking is one of the biggest modifiable risk factors of cardiovascular disease. We know it has negative effects on the body in general but how does it affect our sleep more specifically? When we smoke the effects of nicotine are felt almost immediately, but may take up to 30 minutes for most, and the effects of nicotine wear off within 2-3 hours of consumption. The effects of nicotine consumption are difficulty falling asleep, increased nighttime awakenings, and decreased restorative slow wave sleep and REM sleep causing increased daytime sleepiness.22 These symptoms are more pronounced in individuals who smoke later in the day or closer to bedtime, likely due to nicotine withdrawal occurring while the person is asleep. Additionally, nicotine withdrawal causes increased depression and worsened sleep disturbances which could contribute to smoking relapse, further worsening the sleep disturbances associated with nicotine.22
What about marijuana’s effect on sleep?
Marijuana (and the active ingredient THC) interact with endocannabinoid receptors in the brain to affect sleep. The effects of THC on sleep are dose dependent. THC binds to these receptors and increases adenosine (thereby increasing sleep pressure) as well as enhancing GABA, which is the primary inhibitory neurotransmitter. This can help users fall asleep quicker and increase the amount of slow wave sleep, however this can also lead to dependence on the drug to fall asleep.23 As tolerance develops over time to all drugs, this can lead to higher and higher dosing requirements. Additionally, long term use and higher dose requirements alters sleep architecture by increasing slow wave sleep but suppressing REM sleep (which is why withdrawal leads to vivid dreaming, also our peak testosterone is made during REM sleep), increased brain temperature (opposite of what we want), and a shift circadian rhythm to daytime and diminished sleep quality.23 While short term benefits may exist with marijuana use in sleep, long term changes in sleep architecture and dependence suggests caution.
What about Cannabidiol (CBD) oil and sleep?
Cannabidiol (CBD) oil is in the early stages of being studied for sleep. It is an anxiolytic which is beneficial for sleep, however it appears to have a bimodal effect of causing feelings of alertness at lower doses while at higher doses it is sedating. Further studies need to be done in this area.
How do sleep aids affect sleep?
For those who have issues with sleeping, sleep aides such as Benadryl and Ambien are commonly used to achieve a better night's rest. Benadryl, a common over-the-counter antihistamine containing diphenhydramine, is sometimes used off-label as a sleep aid due to its sedating effects and easy availability. However, its use as a sleep aid is generally not recommended as it can lead to several adverse effects, including daytime drowsiness, dizziness, cognitive impairment, and a heightened risk of falls, particularly in older adults. Additionally, studies have linked the chronic use of diphenhydramine-containing sleep aids with an increased risk of mortality, especially in older individuals.24 Specifically, in regards to cardiovascular health, diphenhydramine has been known to increase heart rate and in higher doses can cause arrhythmias (irregular heartbeats), cardiac arrest, and even death.22 Similarly, prescription sleep aids like Ambien (zolpidem) have also been associated with potential risks including dependency, rebound insomnia once discontinued, impaired driving, and an increased risk of falls, accidents and cardiovascular events. More specifically, a Japanese study showed that use of sleeping pills increases the risk of cardiovascular events in heart failure patients by 8-fold.25 As such, healthcare professionals generally advise against the long-term use of these medications for managing sleep disturbances, emphasizing the importance of non-pharmacological approaches and the careful consideration of risks versus benefits when using sleep aids.
How does melatonin affect sleep?
Melatonin is a hormone that is produced in the pineal gland, and has important effects on the circadian rhythm, as an antioxidant, as a hypothermic (melatonin drops the body temperature by about 1°C which may add to its sleep inducing effects) and in possible immunomodulation and gut microbiome interaction. Light inhibits melatonin production while darkness increases its release. Even indoor light can inhibit this release. Melatonin only helps speed up the onset of sleep, it has nothing to do with sleep quantity or quality overall. In 2022 1.6 billion dollars of Melatonin OTC was sold in the US, including to children. Analysis of this melatonin shows up to 450% higher dosing than is advertised on the bottle, as well as significant variability in dosing between batches from the same company.26 Furthermore, melatonin only increases the speed to sleep by a few minutes (7 minutes in some meta-analysis).27 Given lack of regulation, efficacy and long term chronic use safety data, we do not recommend melatonin except for jet lag and short use cases (4-8 weeks).
How does my sleep environment affect sleep?
The ideal room temperature is 63-68°F. As melatonin levels rise during sleep, our body’s core temperature inversely decreases, therefore, colder room temperatures have been shown to cause increased melatonin release which promotes increased sleep.28 Conversely, studies have shown that increased sleeping temperatures can dysregulate our REM sleep, and cause sleep disruption, whereas cooler sleeping environments have been shown to cause increased N3 sleep, the most restorative stage of the sleep cycle.29 Similarly, it is important to minimize distractions in our sleep environment like loud noises and bright lights as these factors can all disrupt sleep and cause nighttime awakenings.
While natural light exposure during the day is beneficial for regulating the circadian rhythm, exposure to artificial light sources in the evening, particularly blue-rich light, can interfere with the body's internal clock and disrupt sleep and melatonin production. Therefore, reducing exposure to screens and artificial light sources that are high in blue-light, especially in the hours leading up to bedtime, may promote better sleep hygiene and overall sleep health. However, it is unclear at this time whether blue light or just the stimulation from screens disrupt our circadian rhythm. Many have jumped on the trend of blue light blockers, most commonly in the form of screen protectors or glasses. Studies suggest that wearing blue light blockers in the evening does improve sleep quality and increase melatonin levels (although results are mixed).30 Moreover, the engagement with stimulating content on social media platforms can further exacerbate sleep problems by increasing cognitive arousal/awakeness and delaying the onset of sleep (regardless of blue light). Therefore, it is important to reduce screen time 1-2 hours before bed regardless of blue light blocking on not. Furthermore, sleeping in a cold, quiet room will promote a restful night of rest.
How does sleeping with someone else/relationships affect my sleep?
A popular new concept in the sleep medicine world is “sleep divorce”, which is where a couple will sleep in separate beds or bedrooms routinely. According to the American Academy of Sleep, 35% of couples do not sleep in the same bed and 20% will move to a different location.41 Objectively, across multiple studies, sleeping with a partner leads to worsening sleep. However subjectively, partners feel like they get better sleep when sleeping with partners42. The reasons most listed are snoring/sound, partner movement/wake ups, and temperature differences. One solution (without scientific evidence at this point) is the Scandinavian sleep method, where couples use different duvets, separate bedding (that can be connected and allows for individual temperature/mattress control) as well as possibly using earbuds/sound machines to control ambient noise. Of note, sexual activity leading to orgasm (regardless of time of day) leads to vastly improved sleep quality for both men and women, possibly through hormone release (vasopressin for men and oxytocin for women), and/or the change from sympathetic (fight or flight) to parasympathetic (rest and relax) tone post sexual acitivity43.
Does sleep position affect sleep?
While we all move during sleep, most people have a dominant position. Sixty (60%) percent of people are side sleepers, 30% are back sleepers and 10% are stomach sleepers. Side sleeping is associated with better airway management, reduces indigestion (although sleeping on our left may increase reflux) and decreases the symptoms of snoring and sleep apnea.44 During sleep, our brain also washes away metabolites such as beta amyloid and TAU protein (related to Alzheimer’s dementia). In another victory for side sleepers this process is more efficient when people sleep in the side position45. To become a side sleeper, simply get a body pillow, and begin your sleep by lying on whichever side is most comfortable for you. Weighted blankets may also discourage tossing and turning throughout the night.
How does exercise affect sleep?
As we are discussing sleep as it relates to cardiovascular health it is important to consider exercise, one of the biggest promoters of cardiovascular health and fitness. Exercise can have a significant impact on sleep quality and duration, with numerous studies highlighting its positive effects on various aspects of sleep. Regular physical activity, especially aerobic exercise, has been shown to reduce the time it takes to fall asleep.31 Increased activity earlier in the day helps to regulate our circadian clock making us more alert and energized during the day. Furthermore, it promotes the onset of sleep at night, increases sleep depth due to increased tiredness, and decreases the number of nighttime awakenings. Also, exercise can help relieve stress and boost mood, which may improve sleep, as mental health issues are a major contributor to insomnia and sleeping difficulties.31
While the exact mechanisms underlying this relationship are not fully understood, it is believed that the physiological and psychological benefits of exercise contribute to improved sleep continuity and overall sleep duration. Overall, incorporating regular exercise into one's daily routine can lead to numerous benefits for sleep health, including faster sleep onset, improved sleep quality, reduced sleep disturbances, and enhanced overall sleep duration. However, it's essential to avoid vigorous exercise too close to bedtime, as it may have stimulating effects that could interfere with the ability to fall asleep. Therefore, exercise is recommended for earlier in the day, more specifically, mornings for those with circadian disruption.
How does sauna/heat prior to sleep affect sleep?
Similar to exercise, the use of sauna may also promote better sleep through stress reduction, muscle relief, and increased release of endorphins (the hormones involved in increased mood). Heat from Saunas, hot showers or baths initially may delay sleep (see above). However, the rapid decrease in body temperature after exiting is a potent sleep inducer, much the same way as a cold environment is conducive to sleep. Aim for a hot shower/heat exposure 1-2 hours prior to bed.
How does sleep affect eating habits?
Lack of sleep can significantly impact our eating habits and metabolism, leading to changes in calorie intake and levels of important hormones such as leptin and ghrelin. When we don't get enough sleep, our body's internal regulation of appetite and hunger can become disrupted. This disruption often leads to an increase in appetite and cravings for high-calorie, carbohydrate-rich foods. Studies have shown that sleep-deprived individuals tend to consume more calories, particularly from snacks and comfort foods, compared to those who get adequate sleep.32 Leptin, a hormone produced by fat cells, helps the brain to understand when we are full. Similarly, the hormone ghrelin, produced by the stomach, signals to the brain when we are hungry and promotes food intake and hunger.
A lack of sleep disrupts the delicate balance of these two hormones, leading to decreased levels of leptin and increased ghrelin; causing increased feeding and less satiety.33 Furthermore, if this pattern continues, they may also develop leptin resistance which is implicated in obesity. Inadequate sleep can also affect the body's ability to metabolize carbohydrates, leading to insulin resistance and potentially increasing the risk of weight gain and metabolic disorders over time.34 Overall, the interplay between sleep, eating habits, and hormonal regulation underscores the importance of prioritizing sufficient sleep for maintaining a healthy weight and metabolism.
What are the biological mechanisms underlying sleep-related cardiovascular risk?
Numerous biological mechanisms underlie the relationship between sleep and cardiovascular health. Chronic sleep deprivation disrupts neuroendocrine regulation, leading to dysregulation of cortisol, leptin, and ghrelin levels, thereby promoting insulin resistance and obesity, both of which are established risk factors for cardiovascular disease. Additionally, alterations in autonomic nervous system activity, including increased sympathetic tone and decreased parasympathetic activity, contribute to adverse cardiovascular outcomes by affecting heart rate variability, vascular tone, and endothelial function.
In conclusion, sleep exerts profound effects on cardiovascular health, influencing blood pressure regulation, endothelial function, metabolic homeostasis, and overall cardiovascular fitness. Sleep plays a crucial role in modulating blood pressure, hormone levels, body temperature, and restoration of our bodies. Recognizing the intricate interplay between sleep patterns and cardiovascular physiology is essential for implementing effective strategies for cardiovascular disease prevention and management. By prioritizing sleep hygiene, addressing sleep disorders, promoting regular physical activity, and optimizing treatment of cardiovascular risk factors, healthcare professionals can optimize cardiovascular health and improve patient outcomes in both clinical and community settings.
In the last few pages of this section we are going to deal with specific ways to treat insomnia, other sleep related conditions, and give you a step-by-step guide on getting a great nights sleep!
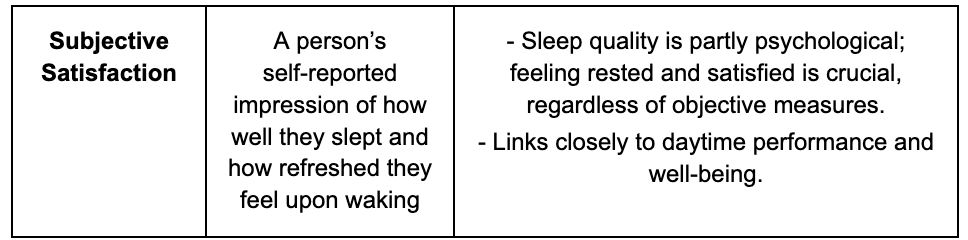
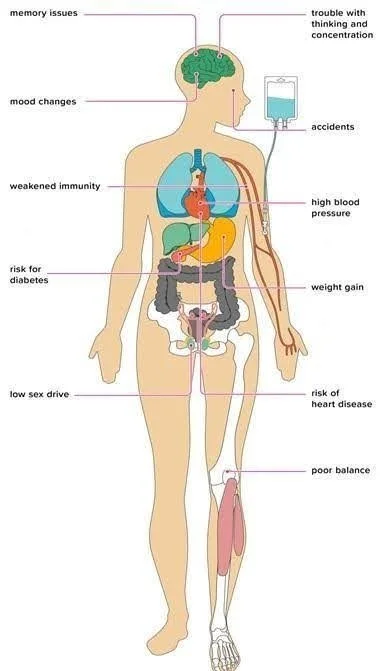
Figure 4. The 11 effects of sleep deprivation on your body. There is no organ that is unaffected by sleep. 35
What is insomnia?
Everyone has one or many bad nights of sleep for a variety of reasons and this is not insomnia. Insomnia can be divided into sleep onset insomnia and sleep maintenance insomnia. Sleep onset insomnia is defined as taking at least 30 minutes to fall asleep, or 30 minutes to go back to sleep, at least 3 nights a week for 3 months in a row37. On the other hand, sleep maintenance insomnia (middle insomnia) is defined as nighttime awakenings at least twice a week for one month that at least moderately impacts your life, but without difficulty falling asleep initially. These two definitions are opposed to sleep deprivation, where you have the ability to fall and stay asleep but don’t have the opportunity (eg. young kids, shift work, etc). Polysomnography (sleep studies) do not aid in diagnosis, the best way to diagnose insomnia is with a test called the insomnia severity index and by keeping a sleep diary for at least 2 weeks.
What causes insomnia?
The 3P model of insomnia states that 33% of insomnia is predisposition (hereditary), 33% is due to precipitating factors eg. social factors such as stress, fighting, rumination, conflict etc, and 33% is attributed to perpetuating factors such as eating or drinking the wrong things (alcohol, caffeine, nicotine etc).36
Why do I wake up at 3 am? What is wrong with my sleep maintenance?
The 3-4 am wake up occurs for several reasons, barring medication, the 3Ps or urinary issues. It is related to our core temperature rising in the setting of waning adenosine levels. Higher late night cortisol from daily stress can also play a role. Imprinting may also occur, where once the body is used to waking up at a set time, it may continue to do so without other stimuli.
The first step in treatment is to explore the tips above and below, ie make sure your sleep routine is robust. Next, hide the clock face so you do not know what time it is ie. You should not know its even 3 am!. You should never sleep with a phone beside your bed. If you do wake up the next thing to do is to take your mind off of it. This is best accomplished with box breathing aka the 4 7 8 technique, where you inhale nasally for 4 seconds, hold for 7 seconds, and breath out for 8 seconds orally, repeating several times46. As always, CBT-I is a cornerstone as well in treating insomnia.
Can you just tell me how to fall asleep and stay asleep consistently?
Reframing sleep from the perspective of circadian biology means treating sleep not merely as an isolated block of nighttime rest, but as a dynamic output of your body’s internal clock. In this view, optimal sleep is achieved by aligning daily behaviors—such as exposure to natural light, meal timing, and physical activity—with your circadian rhythm. For example, receiving ample bright light in the morning helps anchor your internal clock to the day, while reducing blue light exposure in the evening encourages the natural rise of melatonin, facilitating a timely and consolidated sleep period. This approach suggests that consistency in sleep–wake timing and strategic management of environmental cues are key to both sleep quality and overall health.
If you focus on optimizing your sleep based on circadian biology, you will maintain a consistent schedule, maximize morning light exposure, and minimize evening light (especially from screens) to reinforce your natural circadian phase. Including timing of meals, liquids, and substances completes the plan. This strategy is underpinned by robust research demonstrating the precision of the human circadian pacemaker and the potent phase-shifting effects of light. Below are practical tips:
Start the day off with natural bright light exposure. Natural light is preferred but any light input onto your eyes will help alert the body that it is morning. (Note that glass blocks the photons for this light.)
It is better to exercise and eat larger meals earlier in the day, as this helps regulate the circadian rhythm. Specifically, high-intensity exercise leads to increased adenosine levels which will increase sleep pressure and make it easier to fall asleep later.
Avoid long naps during the day since napping will decrease the adenosine levels in your brain, leading to decreased sleep pressure and difficulty falling asleep later.
Napping in increments of 20 minutes has been shown to have the most benefits
Note it is normal to feel tired at the 1-4 pm time frame. This is part of a normal circadian rhythm. There is a theory that we are biphasic sleepers, meaning we were meant to sleep for two periods. We recommend following this chapter’s advice and the midafternoon slump should be kept to a minimum.
Avoid caffeine, nicotine and alcohol at least 4 hours before bed since these substances can make it harder to fall asleep, stay asleep and may disrupt your sleep cycle. If you are sensitive to these substances, you will need to just stop using them.
Decrease bright light exposure at least 4 hours before sleeping to help regulate your circadian rhythm. Try light dimmers (dim to half-light), blue light filters/glasses, and reduced screen time to achieve these effects.
Avoid large meals 2-3 hours before bedtime as they can cause circadian disruption as well as gas, bloating, reflux may interrupt or make it difficult to sleep. Additionally, avoid drinking beverages 1 hour before bed, to decrease nighttime awakenings due to thirst or the need for urination.
The 3,2,1 rule works well here, 3 hours before bed is the last meal, 2 hours is the last electronic use, 1 hour is the last drink (nonalcoholic).
***Caveat*** - if you are too hungry, or if you have trouble getting your protein requirements (1 gm/lbs ideal body weight) then having a high protein (>30 grams) low calorie (<300 kcal) snack can work before bed. Downside would be reflux and/or poor quality sleep47.
Try to limit screens (computers, cell phones and television, etc.) while in bed, the bed should only be used for sleep and intimacy. This helps the brain to associate the bed with sleep and increased sleep onset.
Melatonin supplementation may help in those with circadian disruption, although its effects are not robust. It should not be used long term. Avoid most sleep aids.
Keep the room temperature between 63-68°F, keep the room as dark as possible and minimize noise throughout the night for an ideal sleep environment.
Plan a few minutes for journaling, decompression, meditation etc. Offload the day’s anxieties, end the thought rolodex
Do not stay in bed awake for more than 20-30 minutes; if sleeping is difficult, try getting out of the bed and doing a relaxing activity for 10 minutes, then returning to the bed. Box breath as needed if you wake up.
If you stay in bed awake for a long time (poor sleep efficiency), then compress sleep time (i.e. shift bedtime from 12 AM to 2 am to force sleep pressure). Once you are sleeping 100% of those hours gradually move the bedtime back up.
eg. in bed from 12 am - 8 am but only sleeping for 5 hours? Move sleep time up to 2 am-8 am (efficiency improves to 100%, therefore now getting 6 hours of sleep), then gradually move bedtime earlier in 15 min increments per week.
Try to maintain a regular sleep, light/dark, mealtime and exercise schedule. Keeping these activities as routine as possible entrains your biological rhythms for maximal alertness during the day and maximal sleepiness during the night.
Try to get between 7-9 hours of sleep every night, with the requirement changing depending on your age.
If sleep becomes continuously difficult (see insomnia definitions above), it may be time to see a sleep specialist about a potential sleep disorder. They are fantastic and can offer many treatment options beyond this book such as cognitive behavioral therapy. A list of experts can be found at: https://www.behavioralsleep.org/index.php/united-states-sbsm-members (Society of Behavioral Sleep Medicine)
Key Points
Sleep is crucial for every aspect of health, from metabolism to exercise to longevity. Without adequate sleep it will be impossible to be controlled in other areas.
Learn your chronotype and adjust accordingly
A variety of substances affect sleep in profound and differing ways.
Turning to pharmacology for long term sleep support is a mistake for most patients
Sound sleep starts in the morning. Create a daily routine that makes sleep a priority, so that when you are ready for bed your chances of getting a good night's sleep are maximized.
Sleep in a quiet, cool and dark environment, ditch the screens, have a regular sleep/wake schedule, and do not shortchange the amount of time spent sleeping.